Hypoglycaemia
Contents
- Introduction
- What are the warning signs?
- What causes a hypo?
- How can I treat hypoglycaemia?
- General advice
- Driving
- Useful resources
Introduction
Hypoglycaemia occurs when your blood glucose levels are too low (below 4 mmol/L). This is a potentially dangerous side-effect of some diabetes tablets and insulin. The following advice will help you prevent, recognise and treat a hypoglycaemic episode, commonly known as a ‘hypo’.
What are the warning signs?
Warning signs vary from person to person. However, you will become familiar with your own individual warning signs that your blood glucose level is too low.
Early warning signs
- Headaches
- Shaking or dizziness
- Anxiety or bad temper
- Sweating
- Palpitations
- Hunger
- Tingling lips or fingers
Late warning signs
You may not be aware of late warning signs yourself, but other people may notice you becoming
- moody
- irritable or aggressive
- irrational
- confused
- unable to concentrate
- unable to co-ordinate your movements (e.g. shaking)
- pale
What causes a hypo?
It is important to be aware of what causes hypoglycaemia in order to prevent it. The following are all possible causes:
- Too little or no carbohydrate at your last meal (e.g. no bread, pasta, rice, potato or cereal)
- Missing a meal or eating it later than usual
- Too much insulin or too many diabetes tablets
- Taking more exercise or being more active than usual (e.g. housework, gardening or sport). A delayed hypo can occur several hours after your exercise or activity. Always make sure you have a suitable carbohydrate snack on you when you exercise.
- Alcohol may cause you to have a delayed hypo (overnight or even the next day). Always make sure you have a suitable carbohydrate snack or meal if you drink alcohol.
- Using the same injection site too often which causes lipohypertrophy (fatty lumps). If you change from using an area of lipohypertrophy to using an area of normal skin, you may need to check your blood glucose more often for a while as your insulin requirements may change.
- Direct heat or sauna treatment may cause insulin to be absorbed more quickly and therefore can potentially cause hypoglycaemia.
- Weight loss (whether intentional or not). If you lose weight, then your medication may need to be reduced to prevent hypos.
Occasionally the cause of a hypo may not be obvious. If in doubt, contact your diabetes care team for advice.
How can I treat hypoglycaemia?
The hypoglycaemia flowchart below gives clear advice on what you or the person you are with should do if you experience a hypo.
Mild hypo
If you become aware of any early warning signs then stop what you are doing and treat your hypo quickly by following these steps.
Step 1
Take 15–20 g rapid-acting carbohydrate in the form of ONE of these:
- four or five jelly babies
- 200 ml orange juice
- four to six glucose tablets
Step 2
Recheck your blood glucose in 10 minutes. If it is greater than 4 mmol/L then proceed to Step 3. If it is 4 mmol/L or less then repeat Step 1.
Step 3
To prevent a further drop in your blood glucose, once your blood glucose is above 4 mmol/L after treatment with rapid-acting carbohydrate you should take some medium-acting carbohydrate in the form of ONE of these:
- a biscuit
- a slice of toast
- a piece of fruit
- a glass of milk
- your next meal
Moderate hypo
If you are confused, you may need help from someone else to treat your hypo. If you are conscious, responsive and able to swallow without the risk of choking, your helper should follow the same steps as above, or should treat you with Glucogel.
Glucogel is a tube of gel that raises blood glucose levels quickly. It can be prescribed by your GP or it can be purchased over the counter. Each tube of Glucogel contains 10 g of carbohydrate and so you will need two tubes to treat a hypo.
Glucogel should only be used if the person being treated can swallow. It is vitally important that Glucogel is not given to an unconscious person because of the risk of choking.
A friend, relative or carer should be taught how to use Glucogel as follows:
- Make sure that the person being treated can swallow.
- Twist off the cap of the Glucogel tube.
- Squeeze the tube to insert the gel into the person’s mouth between their teeth and their cheek.
- Rub the outside of their cheek gently to allow the Glucogel to become absorbed. It is absorbed through the lining of the mouth and should help raise the blood glucose within 15 minutes.
You should follow this treatment with a starchy carbohydrate snack such as a biscuit, a slice of toast or your next meal if it is due. You should then recheck your blood glucose level. The treatment can be repeated if necessary.
Severe hypo
If you are unconscious or unresponsive because of hypoglycaemia, this is an emergency situation. You will need immediate attention from another person and/or a healthcare professional. Usually in this situation, your blood glucose will be very low (less than 1–2 mmol/L).
If you are unconscious, someone may need to give you glucagon.
Treating hypoglycaemia with glucagon
Glucagon is a hormone that occurs naturally in our bodies but it can also be produced in a lab and used as a medication. If you use insulin to manage your diabetes, you can arrange for a carer, friend or relative to be taught how to treat a severe hypo by giving you an injection of glucagon. It is branded as GlucaGen Hypo Kit and available on prescription. It raises the blood glucose level by releasing glucose that is stored in the liver.
The person treating you with glucagon should be taught the following step-by-step guide to treat you with glucagon:
- Place the person in the recovery position
- Follow the instruction leaflet that comes with the glucagon and inject the person into a fleshy part of their body, e.g. their thigh.
- Allow around 10–15 minutes for the glucagon to work.
- If the person has not begun to regain consciousness in that time, or if they are showing signs of having a seizure (shaking and/or jerking violently) then call 999 immediately as they may need to have an injection of glucose.
- If the person is regaining consciousness, then recheck their blood glucose level in 10 minutes.
- Once the person is fully conscious and able to swallow, give them a snack of starchy carbohydrate, e.g. a sandwich or slice of toast.
- Continue to monitor their blood glucose level regularly until it is back to within a normal range.
Glucagon may not work if the stores of glucose in your liver are low. This may be the case if you have been drinking a lot of alcohol, if you have eaten very little food or if you had a hypo the previous day.
If you have had any type of hypo, whether mild or severe, always think about what caused it. You can discuss it with your diabetes care team to help reduce the risk of it happening again.
General advice
Here are some tips on how to manage hypos:
- Always carry some form of glucose on you, e.g. glucose tablets or jelly babies.
- Always carry or wear some form of diabetes medical identification, such as a bracelet or wristband, so that people can help you in an emergency. Medic Alert Foundation ID bracelets are recognised worldwide, and can be personalised with information such as your name, details of who to contact in an emergency, and the type of diabetes you have and how you manage it. See https://www.medicalert.org.uk for more details.
- Tell your friends, relatives and colleagues that you have diabetes and let them know how to help you if you have a hypo.
- If you suffer from night sweats or are waking up with a headache you may be having a hypo in the night. If this is the case, you should check your blood glucose in the middle of the night using your glucose monitoring kit.
- You may need to adjust your medication before you exercise in order to prevent a hypo. Your diabetes care team can advise you on this.
- You may have high blood glucose levels for a few hours after a hypo. This can be your body's natural response to a hypo or it may be caused by over-treatment. Discuss this with your diabetes care team.
- If you have a severe hypo, you should always inform your diabetes team.
What if I have a hypo when I'm due to have my insulin injection?
- Take some rapid-acting carbohydrate.
- Once your blood glucose level is above 4 mmol/L, take your insulin as normal. Occasionally it may be better to take a slightly smaller dose, particularly if there is no obvious reason for the hypo.
- Have your meal without delay.
- Talk to your diabetes care team as soon as you can, especially if you have frequent hypos or are experiencing them more often. Your insulin dose may need to be adjusted. If you are experiencing more than one or two mild hypos a week, then you should definitely ask for advice.
- You should never miss an insulin injection.
What if I have a hypo when I'm due to have my insulin or tablets?
If this happens, then follow these steps:
- Take some rapid-acting carbohydrate.
- Once your blood glucose is above 4 mmol/L, take your tablets or insulin as normal.
- Have your meal without delay.
- Talk to your diabetes care team as soon as you can, especially if you have frequent hypos or are experiencing them more often. Your medication may need to be adjusted. If you are experiencing more than one or two mild hypos a week, then you should definitely ask for advice.
Driving
- Always carry some form of glucose in the car, e.g. glucose tablets or jelly babies.
- Check your blood glucose level before you drive and do not drive if your blood glucose is less than 5 mmol/L (an easy way of remembering this is: ‘Below Five, Do Not Drive’).
- If you have a hypo when driving, stop the car as soon as it is safe to do so.
- Take fast-acting carbohydrate immediately.
- Remove the key from the ignition and move into the passenger seat.
- Ensure that your blood glucose level is above 5 mmol/L for 45 minutes prior to driving again.
Useful resources
The following Hypo flowchart will let you see at a glance how to treat a hypo, depending on how severe it is.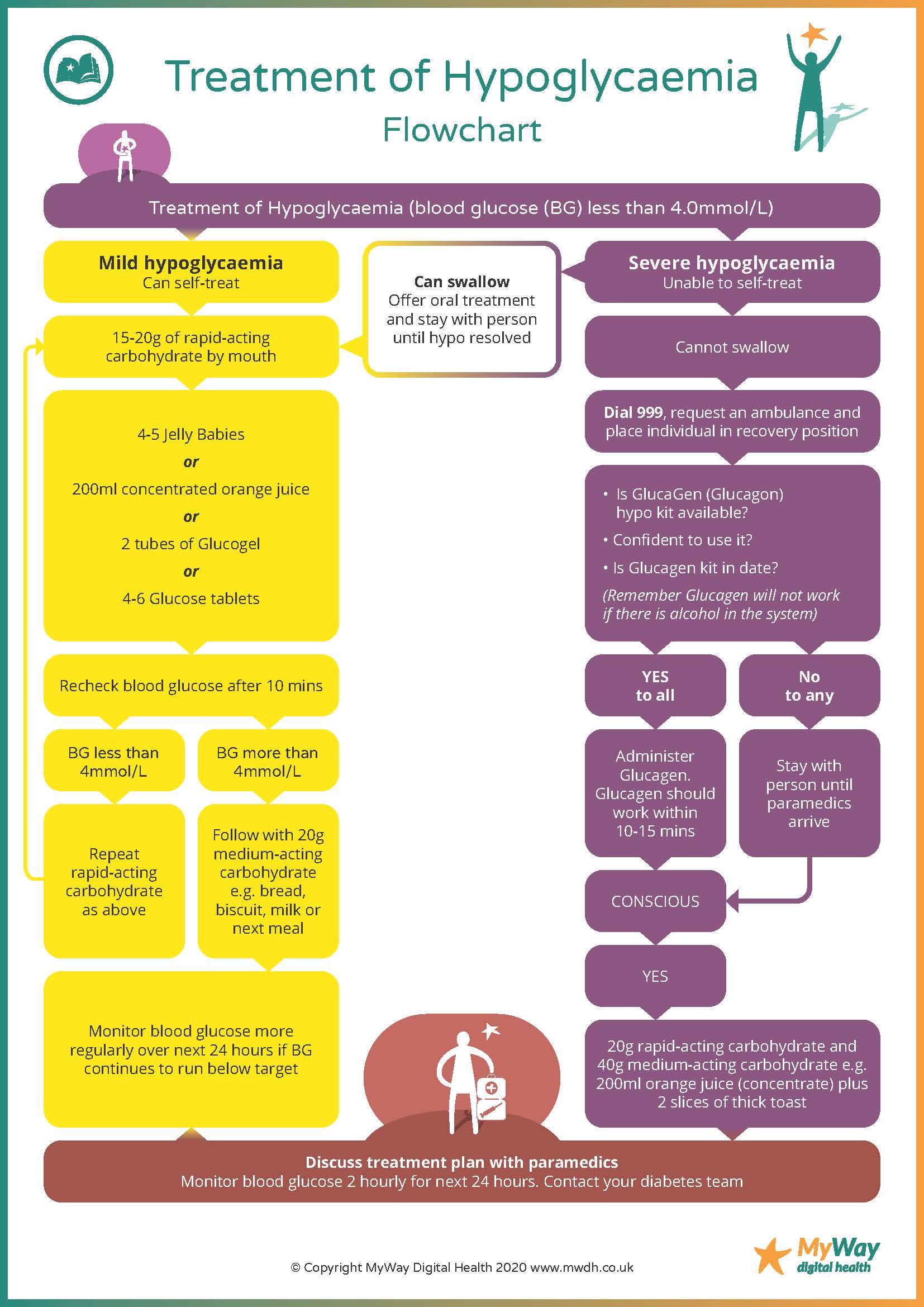
This guide is intended for use when you are generally well.
For information on ‘sick day guidance’ for type 1 diabetes, click here.
For information on ‘sick day guidance’ for type 2 diabetes, click here.
For more information on the treatment and prevention of hypoglycaemia click here.