Why is my blood glucose high?
A variety of factors can cause an increase in blood glucose levels in people with diabetes. If you’ve been experiencing high blood glucose levels, some common things that may be affecting them are:
- Injection site issues
- Injection technique
- Issues with insulin pumps:
- Blockages/occlusion
- Bubbles in insulin pump
- Loose infusion site
- Insulin issues:
- Out of date
- Too warm
- Mismatch with insulin to carb content
- Change in your diet
- Change in the environment:
- Cold weather
- Hot weather
- Changes in physical activity levels
- Emotional stress
- Starting a new medication, e.g. steroids
- Short-term illness
- Other conditions
Injection site
Injecting insulin into the same site regularly can lead to fatty lumps forming on the surface of the skin which you may find unpleasant, and it can also affect the rate at which insulin is absorbed, This is commonly known as lipohypertrophy and is the result of extra fat being produced at that part of the body.
Insulin isn’t delivered consistently when you inject into an area of fatty lumps, which means that insulin can take longer to be absorbed leading to higher blood glucose levels, or it can be absorbed too quickly, leading to low blood glucose levels.
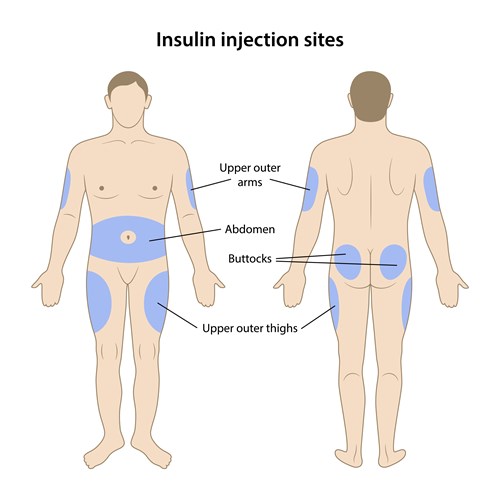
To prevent this, make sure you rotate your injection sites. Good sites are areas where there is a decent layer of fat such as the stomach, upper arms, buttocks or thighs. It’s important to note that different areas of the body absorb insulin quicker than other parts. The stomach is the quickest to be absorbed, followed by the upper arm, the thighs and lastly the buttocks.
Injection technique
Your injection technique is important, and it can make a big difference to your blood glucose levels for several reasons:
- Longer needle length: Using a needle longer than 4mm can lead to insulin being injected into the muscle, rather than the fatty (subcutaneous) layer. This will lead to the insulin being absorbed more quickly.
- Lifted fold in the skin not performed correctly: Very slim adults or children may need to inject into a pinched fold of skin. Injecting into folded skin ensures that you inject into the fatty layer, rather than the muscle.
- Needle withdrawn too quickly: If you withdraw the needle too quickly it means that the full dose of insulin won’t be delivered and may result in high blood glucose levels. You should hold the needle in for at least 10 seconds after the dose has been injected to make sure all of it has been delivered.
- Cloudy insulin hasn’t been mixed correctly: Cloudy insulins such as NPH (Neutral Protamine Hagedorn) or premixed insulin need to be gently rolled and inverted ten times each before being injected. The solution will turn milky white as the crystals go back into suspension.
- Never reuse needles: Syringe or pen needles should only be used once. Reusing a needle can cause damage to it, which will not optimise insulin delivery. There is also an association between needle reuse and lipohypertrophy (fatty lumps).
- Check pen and needle: To make sure both the pen and needle are working correctly, dial 2 units on the dose button and hold the pen with the needle pointing upwards. Press the dose button to make sure you can see insulin appear on the needle tip.
-
To read more about this, have a look at our injecting insulin resource.
Issues with insulin pumps
There are a few issues with insulin pumps that may prevent optimal insulin delivery and cause high blood glucose levels. If you are finding that your levels are high, it’s worth checking the following:
Blockage/Occlusion: An occlusion is another word for a blockage in your pump that prevents it from delivering insulin. Most pumps sound an alarm to let you know about a blockage. Common reasons for this are:
- The cannula being bent during insertion
- A kink in the insulin pump tubing
- Crystals forming in the insulin
- Pressure to the tubing or insertion site
Check to make sure you can see no obvious signs of a blockage or that the cannula has bent and needs to be replaced. You may need to change your infusion site if insulin delivery is still impaired. If you are suffering frequent blockages speak to your diabetes care team.
Bubbles in insulin pump:
If there are air bubbles in your insulin pump you won’t get your full insulin dose which can lead to high blood glucose levels. The most common reasons for air bubbles are:
- Not priming the air out of the reservoir when refilling the reservoir or putting in a new cartridge
- A loose connection in the tubing
- Not priming the air out of the tubing when changing to a new infusion set
- Using insulin straight out of the fridge – as it warms up to room temperature air bubbles can form
Dealing with bubbles varies across different manufacturers but the general advice is to take care when priming your pump to remove air from the reservoir and tubing, make sure there are no loose connections and use insulin that is at room temperature in your pump.
Infusion sites becoming loose
This is a common issue and can occur if sweat is gathered at the infusion site which can cause the cannula to break free. The adhesive on the infusion site should be well secured to the skin, so if you find that it is lifting at the edges, it needs to be replaced straight away. You may find that applying an adhesive like a Skin Grip patch or a Tegaderm dressing to help it stick better.
To read more this, have a look at our insulin pump resource.
Insulin issues
Out of date: You shouldn’t use insulin past the date of expiry as it will not work as effectively. All insulin should be discarded past the expiry date even if some of the solutions remain. Insulin that you are not using should be stored in the fridge but never in the freezer.
Temperature: Insulin is affected by extreme cold or heat, which includes direct sunlight. If you are finding that your blood glucose levels are higher than you expect on a hot day, it might be that the sun has damaged the insulin, so it doesn’t work as well. In hot weather, you should keep insulin in a cool such as a Frio insulin wallet or a Medicool bag. Clear insulin turns cloudy when damaged by the heat, cloudy insulin can become grainy and can stick to the side of the glass. If insulin has been damaged by direct sunlight, then it may turn a brown colour. If you think your insulin has been damaged, then you should not use it.
Insulin dose to carb content mismatch
The role of insulin in the body is to allow our body to use the glucose that is produced from the carbohydrates we eat, to provide energy to our cells. In this way, insulin regulates the levels of glucose in our blood which is why it is important to match the amount of insulin you take with the carbs you eat.
Too much insulin to carb ratio can cause your blood glucose levels to go too low, not enough insulin can cause them to be too high. The number of units of insulin you take for a set amount of carbs can vary from person to person. Speak to your diabetes care team to work out your personal insulin-to-carb-ratio. You can also have a look at our carbohydrate counting resource or the TREND UK leaflet on managing mealtime insulin for further information.
Change in diet
Changing what you normally eat can result in some variance in your blood glucose levels. It may be due to not knowing the exact amount of carbs and overestimating the amount of insulin to take. Alternatively, if carbs are eaten with fat, the rise in blood glucose levels can be much slower, meaning you may need to delay or split the insulin dose to compensate. When trying new foods or changing your diet it is helpful to keep a log of your food and insulin so you can measure the impact on your blood glucose levels. This will help you, over time, become more accurate in matching your food to insulin ratio.
Weather/Climate
Not only can extreme changes in temperature affect insulin, but it also has an impact on your diabetes control. Long periods of lying in the sun can cause your blood glucose levels to rise. Insulin is also absorbed more quickly from the injection site in warm weather which can increase the risk of hypos.
Cold weather can also have an impact on your blood glucose levels. Winter is a time when you’re more likely to pick up an illness which can make your body more resistant to insulin. This means your blood glucose levels can rise and you may need to increase your insulin dose. Have a look at our sick day guidance for type 1 and type 2 for further information.
In both hot and cold weather, general advice to follow is to test your blood glucose levels more frequently and drink plenty of fluids.
Changes in physical activity levels
Physical activity is good for your health and all types of diabetes but changes in your activity levels can have an impact on your blood glucose levels. If you are normally very active, then you might be used to eating more carbohydrate and taking a corresponding insulin dose to match this carb intake. If you have an injury and can’t exercise as you normally would, you will need to adjust your carbohydrate intake and insulin dose.
Competitive sports or high-intensity activities such as sprinting or weightlifting can also cause your blood glucose levels to rise due to the impact of other hormones. When you compete in exercise it can cause your body to become stressed and nervous which prompts your body to produce the hormones adrenaline and cortisol, which in turn can increase your blood glucose levels.
To read further about the impact of exercise on blood glucose levels then please click here.
Emotional stress
Stress causes your body to release stress hormones, like cortisol and adrenaline, which puts your body into a ‘flight or fight’ response. This biological response is to give your body a burst of energy to deal with the perceived threat. These hormones make it harder for insulin to work properly and, as the energy is unable to fuel your cells, it causes your blood glucose levels to rise.
If you continue to feel stressed it can keep your blood glucose levels raised which can put you at risk of developing diabetes complications. Stress can also affect your mood and how you look after yourself.
Diabetes can cause stress in itself, particularly if you’ve just been diagnosed, as you may worry about what you’re eating, how much insulin you need to take, trying to avoid going too low or too high – there are a lot of things to think about. Speak to your diabetes care team if you’re feeling overwhelmed or anxious, or you can have a look at the support pages on the Diabetes UK website. Remember you are not alone with this and many others have felt the same way.
Starting a new medication
Some medications that you get with a prescription and some you can buy over the counter can cause your blood glucose levels to increase. These include:
- Steroids (also called corticosteroids) which treat inflammatory diseases such as arthritis, lupus and allergies.
- Medications that treat anxiety, depression, ADHD and other mental health conditions. Examples include clozapine, olanzapine, risperidone and quetiapine.
- Birth control pills.
- Drugs that treat high blood pressure such as beta-blockers and diuretics.
- Statins, which are used to lower cholesterol levels.
- Adrenaline, which is used to treat severe allergic reactions.
- Some acne medications such as isotretinoin.
- Some anti-rejection drugs such as tacrolimus.
- Medications that are used to treat HIV and hepatitis C.
- Decongestant medications such as pseudoephedrine which can be found in some cold and flu medicines.
- Cough syrup.
- Niacin, which is a B vitamin.
Although these medications can raise your blood glucose levels, it doesn't mean that you shouldn't take them if you need them. Make sure that you consult with your doctor or diabetes care team before taking any new medicines or changing medicines, even if it is for something minor such as a cough or cold.
Your doctor and diabetes care team must know all of the medications you take, both for diabetes and any other conditions. They can then advise you of the best way to take it and whether you need to do anything further such as testing your blood glucose levels more frequently.
Short-term illness
When you’re ill your body become more resistant to insulin. This means your blood glucose levels can rise and you may need to increase your insulin dose. It’s important to test your blood glucose and ketone levels more frequently and to follow the sick day guidance for type 1 and type 2 diabetes.
You should never stop taking your insulin when you are ill. If you are vomiting and are unable to eat, then keep sipping fluids to prevent dehydration. If you are unable to keep fluids down and can’t reduce your blood glucose and ketones level, then you need to seek medical assistance immediately.
Other conditions
Other conditions can have an effect on your blood glucose levels which can make your diabetes more difficult to manage. Diabetes, in turn, can also increase your risk of other conditions.
If you are still experiencing high blood glucose levels after considering everything else mentioned in this resource, then you should speak to your doctor or diabetes care team about it.